
This article covers everything you need to know about strep throat symptoms in adults and children, what causes strep throat, how you get it, how to prevent infection, and red flag signs that indicate you need to see your doctor immediately.
Strep throat is caused by bacterial infection of the throat and tonsils by Streptococcus pyogenes, a gram-positive bacterium also known as group A streptococcus (GAS).
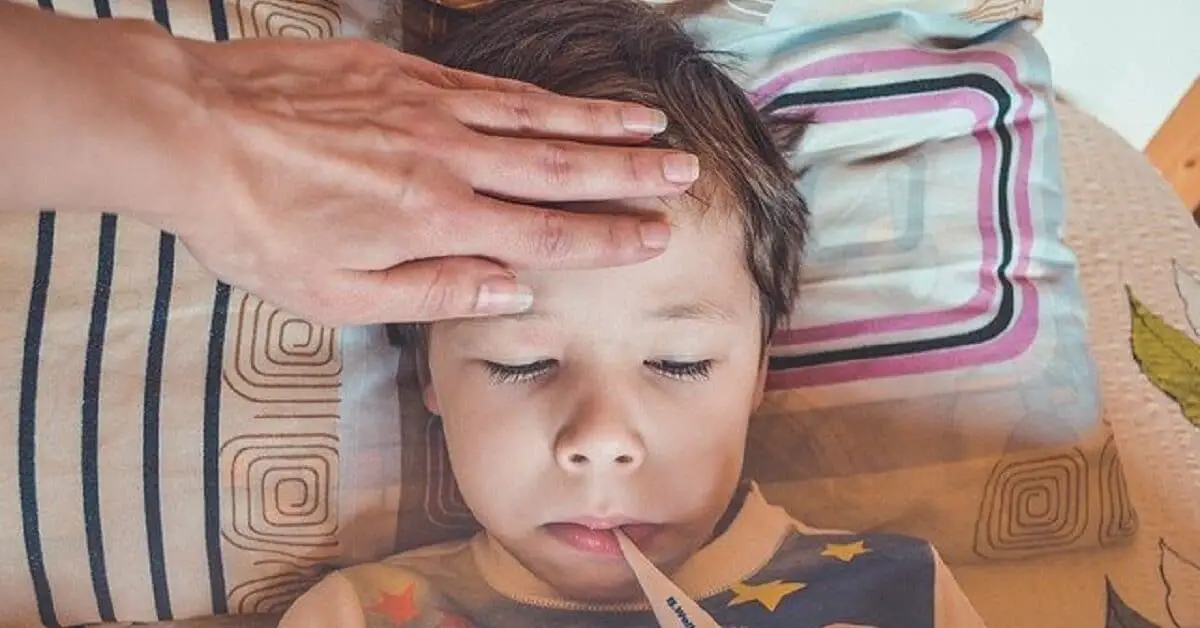
GAS infection of the throat causes inflammation and pain (sore throat). Anyone can become infected, but it is more common among school-age children (5-15 years), according to Dr. Moyo Adeyemi, FRCPC, a pediatrician and CARE healthy living Medical Advisor.
Strep throat — also known as streptococcal sore throat or streptococcal pharyngitis — is a highly contagious disease. It spreads quickly in places, such as schools, where many people are gathered or crowded together.
How do you get strep throat?
People with strep throat may have symptoms or remain asymptomatic. Both symptomatic and asymptomatic people who have the germs in their nose and throat spread it through infected respiratory droplets, saliva, or nasal secretions. They spread it when they talk, cough, sneeze or kiss.
However, people with symptoms tend to be more contagious than asymptomatic carriers.
Although less likely, the infection may also spread through contact with infected surfaces, such as tabletops or objects (fomites), such as computer keypads and toys. You may get group A strep infection when you touch a surface contaminated with droplets from an infected person’s nose and throat and then touch your nose, mouth, or eyes with your fingers.
You may also get strep by sharing eating and drinking utensils (spoons, cutlery, cups) with infected persons or through contact with fluid from strep skin sores (impetigo). Occasionally, the infection may spread through food contaminated (foodborne infection) as a result of improper handling, according to CDC.
People are the primary carriers and spreaders of the infection. There is no evidence it is spread to humans by household pets, such as dogs and cats.
Strep throat symptoms in children and adults

We previously discussed the symptoms of pneumonia in children and adults, and the symptoms of multiple sclerosis (MS) in women.
Here we offer an in-depth exploration of strep throat symptoms in adults, children younger than 3, and school-age children (5-15 years old). We shall discuss the causes and risk factors of strep throat and the differences between bacterial and viral pharyngitis (pharyngitis refers to sore throat caused by inflammation; strep throat is an example of bacterial pharyngitis).
We shall also explore other types of infections caused by group A streptococcus (GAS) and complications that may arise due to GAS infection in children and adults.
Early strep throat symptoms
Strep throat symptoms usually develop 2 to 5 days after exposure to the infection.
Although the severity of strep throat varies from person to person, it is generally a mild infection, and many healthy people recover within a week without treatment. But some may need antibiotic treatment to overcome the infection.
Strep throat is considered a mild, non-invasive infection when it doesn’t spread and damage other organs. However, the pain caused by strep throat can become very uncomfortable, especially for young sufferers who may lose their appetite and refuse to eat and drink.
If left untreated, strep throat may lead to serious complications, such as rheumatic heart disease or kidney problems. Thus, it is important to know the early signs and symptoms and seek prompt medical attention when you believe you or your child may have the infection.
“Strep throat is quite common in children, especially between 5-15 years,” Dr. Adeyemi, FRCPC, told our reporter. “More important are the sequelae that can affect the heart and kidneys. The heart sequelae are the most worrisome. [The sequelae are] the reason why we treat [strep throat] as it could be self-limiting.”
“There was an outbreak of kidney disease sequelae of strep throat in Northern Manitoba a few years ago,” Dr. Adeyemi said. “Thankfully, most of the children had good outcomes. I had two heart sequelae that I can remember.”
“Parents must get their children to see a doctor when they have throat infections, ” she continued. “Most often, it’s viral, but your doctor must determine it isn’t strep throat.”
Sore throat is usually the first sign of infection. The pain occurs without a cough, and you feel it when you try to swallow. You may also have a fever.
Below is a summary of the signs and symptoms of strep throat, according to CDC:
- Sore or painful throat on swallowing (odynophagia) that has a sudden or rapid onset
- Difficulty swallowing (dysphagia)
- Fever and chills that start suddenly or abruptly and develop quickly
- Reddening of the pharynx and tonsils (pharyngeal and tonsillar erythema)
- Inflammation of the tonsils (swelling or tonsilar hypertrophy) and pharynx with or without white patches and exudate (pus or fluid secreted due to infection and inflammation)
- Petechiae (small red spots) may be visible on the soft or hard palate (roof of the mouth)
- Swollen and tender lymph nodes in the neck (cervical lymphadenopathy)
- Headache
- Body aches and pains
- Fatigue or weakness
Strep throat symptoms in children aged 5 to 15 years
In addition to the early strep throat symptoms listed above, school-age children 5 to 15 years may also have:
- High-grade fever (scarlet fever)
- Scarlet fever rash (scarlatiniform rash) may be one of the early symptoms of group A strep infection in children
- Strawberry tongue (reddish tongue with a white coating) and flushed face are other signs of scarlatina
- Stomach pain
- Nausea
- Vomiting
- Anorexia: Loss of appetite; refusal to eat or drink may exacerbate fatigue and weakness and lead to weight loss or emaciation
Symptoms of strep throat in children younger than 5
Strep throat is generally uncommon among non-school-age children younger than 5. It is also rare among infants and toddlers younger than 3. But when it occurs, the symptoms are usually different than in older children and rarely include the typical symptoms of acute group A strep pharyngitis, according to CDC.
The symptoms of strep throat in children younger than 5 years may include:
- Mucopurulent rhinorrhea refers to thick, colored, and opaque nasal discharge
- Fever
- Irritability,
- Anorexia (see above)
- Subacute fever (high-grade fever is rare)
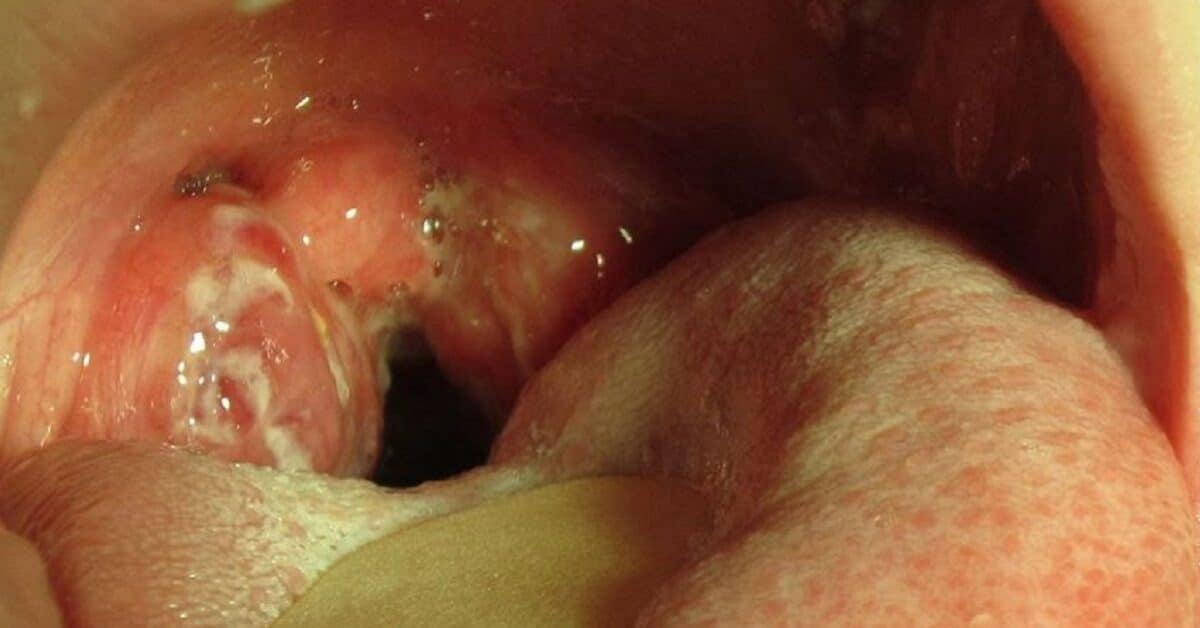
What does strep throat look like?
The images below show what strep throat looks like. The first shows inflammation of the pharynx and tonsils with white patches and exudate. The second image shows petechiae (small red spots) on the soft palate, while the third shows inflamed tonsils with exudate.
The fourth image shows tonsillar exudate in an 8-year-old with strep throat.



Strep throat vs. viral sore throat

Group A streptococcus causes strep throat. However, viruses, such as common cold viruses (rhinoviruses, coronaviruses, adenoviruses), influenza, and Epstein Barr virus (EBV), are the most common causes of sore throat. Viruses cause more cases of pharyngitis than bacteria in all age groups.
Studies estimate that group A strep is the most common bacterial cause of pharyngitis, but it accounts for only 20%-30% of all cases of pharyngitis in children, and about 5%-15% of pharyngitis infections in adults (Ashurst and Edgerley-Gibb).
Doctors often need to differentiate viral pharyngitis from bacterial pharyngitis through the patient’s history, symptoms, and clinical examination. Symptoms that suggest that a case of pharyngitis is viral and not bacterial include:
- Cough
- Nasal discharge or runny nose (rhinorrhea)
- Mouth (oral) ulcers
- Hoarseness
- Pink eye (conjunctivitis)
Symptoms of group A strep don’t usually include cough, nasal discharge (rhinorrhea), hoarseness, oral ulcers, or conjunctivitis. So, the occurrence of these symptoms is usually suggestive of a virus-caused sore throat.
More serious conditions such as cancer tumors and a rare life-threatening condition called epiglottitis (inflammation of upper airways that may cause respiratory arrest) may also cause sore throat. You may also have a painful throat due to allergies, pollutants, chemical irritants, and irritation due to dry, hot, or cold air.
Group A streptococcal diseases: Invasive GAS infections

Strep throat is only one of many infections caused by group A streptococcus. The infections caused by the pathogen are classified as superficial (strep throat, scarlet fever, impetigo), invasive (cellulitis, sepsis, necrotizing fasciitis, streptococcal toxic shock syndrome), and post-infectious immune-mediated complications of strep throat (rheumatic fever, rheumatic heart disease, post-streptococcal glomerulonephritis) (Barth et al.; Barnett et al.).
Invasive and immune-mediated infections are more severe forms of GAS infection and usually occur as complications of strep throat. GAS infection is considered invasive when it invades other tissues and organs, such as the blood, muscle tissues, or lungs.
The incidence of serious GAS infections has decreased in developed countries, but it remains a public health problem worldwide. GAS infections are common among people living in overcrowded and unsanitary conditions in developing countries and among poorer people in some developed countries.
In the 1980s, genetic changes in circulating group A streptococcus strains led to the emergence of new and more virulent strains that caused an upsurge in the incidence of infections worldwide, including the U.K. and northeast Asia (Barnett et al.)
According to the CDC, the WHO reported that 111 million children living in developing countries have impetigo (a skin condition caused by GAS). About 470,000 new cases of acute rheumatic fever (a severe GAS disease) and 282,000 new cases of rheumatic heart disease occur each year.
WHO stats also revealed that about 15.6 million persons worldwide have rheumatic heart disease. GAS diseases rank in the top 10 infections that cause human deaths worldwide (Barnett et al.).
Carapetis et al. reported at least 18.1 million cases of severe GAS infections worldwide. The authors estimated about 1.78 million new cases of GAS diseases and 517,000 deaths each year.
Rheumatic heart disease is the most prevalent of severe group A streptococcus disease with at least 233,000 deaths each year.
Strep throat: Causes and risk factors
The risk factors of strep throat include:
1. Age
Strep throat can affect people of all ages, but children are more likely to get infected and develop the illness.
The infection is uncommon among children younger than 3 years old, but most common among school-age children aged 5 to 15 years. Generally, it is more common in young people less than 18 years.
Among adults, the incidence is higher in people younger than 40 and declines steadily (Ashurst and Edgerley-Gibb).
Adults are less susceptible to strep throat, but those who live or work in close contact with children are more likely to get it. These include parents of young school children, their caregivers, teachers, pediatric hospital staff or children’s clinic staff.
Strep throat is also more common during winter and early spring when people live indoors in close contact with each other.
2. Crowding
Group A strep infection spreads quickly in crowded places because it is transmitted from person to person through contact with saliva, nasal secretions, and respiratory droplets. The infection spreads quickly at places where children gather in groups, such as daycare centers, nurseries, and schools. It may also spread in military barracks and among poor people exposed to crowded and unsanitary conditions.
3. Nutrition
Guevera et al. reported that epidemiological data suggest vitamin D deficiency is associated with an increased risk of infection with streptococcal bacteria. Nseir et al. also reported an association between vitamin D levels and recurrence of strep throat in adults.
Invasive group A streptococcal (GAS) disease risk factors
Factor et al. reported that the following factors were associated with invasive group A streptococcal disease in children and adults:
- Three or more persons living in a home (crowding increases the risk of GAS infection)
- A child living in the home (children are most likely to introduce GAS infection to their home and infect older relatives)
- Smokers living in the home
- Chronic obstructive pulmonary disease (COPD)
- Cardiac disease
- Diabetes mellitus
- Cancer
- Paralysis
- Use of NSAIDs, corticosteroids, and injecting drug use
- HIV infection in adults
- Varicella-zoster virus (VZV) infection in children
Strep throat complications

Strep throat is considered a mild infection (Al-Hamad). When left untreated, the symptoms of the infection are often self-limited and many patients recover in days. However, in some cases, serious complications may develop when the infection spreads to other previously unaffected parts of the body.
We noted earlier that invasive and immune-mediated GAS diseases usually occur as complications of strep throat.
Al-Hamad classified the possible complications from group A strep infection as suppurative (invasive) tonsillopharyngeal (relating to the tonsils and pharynx) complications and non-suppurative immune-mediated complications.
Although the incidence of these complications decreased dramatically in developed countries due to improved living conditions and the introduction of effective antibiotics, they remain significant health problems. The CDC reported that about 11,000 to 24,000 cases of invasive GAS occur in the U.S. each year, with 1,200-1,900 people dying.
Suppurative (production or discharge of pus) complications of group A strep pharyngitis (Ashurst and Edgerley-Gibb; Al-Hamad) include:
- Tonsillopharyngeal cellulitis and abscess: Tonsillar cellulitis refers to the spread of infection from the tonsils and pharynx deeper into surrounding tissues. Abscesses (pockets of pus) may develop near the tonsils (peritonsillar abscess or quinsy) or in the side of the neck (parapharyngeal abscess) due to bacterial infection
- Necrotizing fasciitis (flesh-eating disease) refers to a fast-spreading inflammatory primary infection of the fascia (the fascia is the connective tissue below the skin that holds other tissues and organs in place) and secondary infection of surrounding skin, soft tissues, and muscles that leads to necrosis (death) of muscle fascia and subcutaneous tissues; may end fatally due to sepsis, shock, and multiorgan failure if not promptly treated
- Sinusitis: Inflammation due to infection of the tissues lining the sinuses (the sinuses are small air-filled spaces in the forehead near the eyes and on both sides of the nose near the cheekbones)
- Ear infections: Otitis media or middle ear infection
- Mastoiditis is an infection of the mastoid, the skull bone behind the ears
- Bacteremia: Infection may also spread to the bloodstream
- Meningitis is inflammation of the membranes covering the brain and spinal cord due to infection
- Cerebral abscess: A pocket of pus in the brain
- Jugular vein septic thrombophlebitis is a life-threatening complication of tonsillar infection characterized by painful inflammation of the wall of the jugular vein associated with thrombosis (blood clot) and bacteremia (Lemierre’s syndrome)

Non-suppurative immune-mediated complications of GAS pharyngitis include:
- Scarlet fever
- Acute Rheumatic fever (ARF) and rheumatic heart disease (RHD) are inflammatory complications that affect the joints, nerves, skin, and heart, and may cause damage to the heart valves
- Acute poststreptococcal glomerulonephritis is a rare inflammatory disease of the kidneys that develops after GAS infection
- Poststreptococcal reactive arthritis (PRSA) is arthritis that develops after GAS infection
- Streptococcal toxic shock syndrome (STSS) is a rare but potentially fatal condition caused by the spread of bacteria into deep tissues and the bloodstream
- Poststreptococcal autoimmune dystonia (dystonia is a movement disorder in which muscles contract involuntarily) associated with striatal necrosis (striatal necrosis is a neurodegenerative disease affecting certain brain structures)
- Guttate psoriasis is an autoimmune skin condition common in children, characterized by small, red, and scaly teardrop-shaped spots that appear in the limbs and torso
- Sydenham’s chorea is a neuropsychiatric disorder characterized movement disorder (chorea) alongside psychiatric symptoms, such as emotional instability, attention deficit, and compulsions; it is believed to be caused by an autoimmune response to GAS that affects the basal ganglia (a brain structure); it is more common in girls than in boys
Strep throat complications in children: Rheumatic fever risk factors
Children and teenagers are more likely than adults to develop rheumatic fever after strep throat. Rheumatic fever is partly an autoimmune response to group A strep infection characterized by fever and inflammatory involvement of multiple organs, including the heart (rheumatic heart disease), joints, and central nervous system.
Rheumatic heart disease manifests as carditis (inflammatory disease of the heart) and may lead to damage to the heart valves (mitral and/or aortic valves). Thus, it is important to diagnose and promptly treat strep throat in individuals at a higher risk of rheumatic fever.
Although the exact relationship between strep throat and rheumatic fever remains unclear, there is a higher risk of the fever in cases where strep infection is not properly treated with antibiotics and, therefore, not completely cleared from the pharynx (Al-Hamad).
According to the CDC, other risk factors include a history of rheumatic fever. People who have had the fever in the past are more likely to have a recurrence if they develop strep throat again. The incidence of the disease is higher among children aged 5 years to 15 years and rare in children younger than 3. It is also rare among adults who never had the fever when they were children.
People living in crowded conditions also have an increased risk of developing the disease.
Early diagnosis of strep throat and treatment with appropriate antibiotics greatly reduces the risk of developing rheumatic fever and other complications of strep throat. Early treatment with effective antibiotics also shortens the duration of strep throat symptoms and reduces the likelihood of transmission to close contacts, including classmates, and family, according to CDC.
Some researchers have suggested a link between group A strep and a rare autoimmune condition known as pediatric autoimmune neuropsychiatric disorder associated with group A streptococci (PANDAS).
The condition is characterized by symptoms of obsessive-compulsive disorder (OCD) and tic disorder (involuntary twitching, movements, and sounds) that appear after strep throat or scarlet fever.
Strep throat treatment: When to see your doctor
Strep throat red flags that indicate that you or your child need to see a doctor immediately include:
- Persistent sore throat and tender lymph glands: See your doctor if there is no improvement in symptoms after being on doctor-prescribed medication for more than two days
- Severe and unremitting pain in the throat
- When a child stops eating and drinking due to pain and swallowing difficulties
- Rigors, shaking chills, persistent fever greater than 102°F (39°C), and night sweats
- Swelling in the neck or throat indicative of peritonsillar or parapharyngeal abscess
- “Hot potato” voice
- Rash indicative of scarlet fever
- Drooling
- Trismus: Spasm of the jaw muscles may lead to restricted range of motion of the jaws.
- Sore throat with breathing difficulties (apnea)
- Dark-colored urine (“coca-cola urine”) suggestive of kidney involvement
- Weight loss
- People who are immunocompromised must seek prompt medical attention
Strep throat prevention
There is no vaccine to prevent strep throat so it is best to prevent the infection through strict hygiene and sanitation.
You need to avoid getting strep throat infection because a single infection does give you immunity against a second and third infection. Repeated infections increase the risk of complications.
Hygiene and sanitation involve practices that protect you and others from getting the infection.
- Avoid crowds if possible
- Practice social distancing to avoid being infected by respiratory droplets from other people
- Wash your hands with soap and warm water regularly
- You may also disinfect your hands with alcohol-based sanitizers
- Avoid touching your nose, mouth, and eyes with your fingers, especially after being in contact with possibly infected people or touching possibly infected surfaces and objects
- Avoid spreading the infection by covering your mouth and nose when you cough or sneeze
- Avoid sharing unwashed cups and utensils with people who may be infected
- Good nutrition
- Regular exercise
- Avoid smoking
- Get plenty of rest and sleep
- Isolate (that is, stay away from school or work) if you have strep throat
Strep throat treatment: A note to our readers

Although this article is based on information from peer-reviewed studies, reputable professional health organizations, and trusted public agencies, it is meant only for informational purposes and not in place of advice and care by qualified medical professionals.
We, therefore, strongly recommend that you consult your healthcare provider if you believe you or your child is showing symptoms that may be due to strep throat.
Your doctor will ask you about your symptoms and conduct a physical examination. He may also order tests, such as rapid antigen detection test (RADT) or throat culture, to determine whether your infection is due to group A strep infection.
A throat culture is considered the gold standard diagnostic test for group A strep (Gerber et al.). CDC recommends antibiotic therapy for all patients with positive RADT and throat culture, but viral pharyngitis should not be treated with antibiotics.
Thus, If your doctor determines that you have strep throat he may prescribe antibiotics.
Penicillin or amoxicillin are the antibiotics of choice, according to Shulman et al. However, in cases involving penicillin/amoxicillin-resistant pathogens or penicillin allergy, your doctor may prescribe other effective antibiotics, such as cephalosporins (cephalexin, cefadroxil), azithromycin, clarithromycin, and clindamycin.
Patients recovering from group A strep need plenty of rest, plenty of fluids, and good nutrition.

