Pneumonia is an inflammatory disease of the lungs caused by infection with various pathogens, including bacteria, viruses, and fungi. The common symptoms of pneumonia are due to inflammation of the alveoli following infection of one or both lungs.
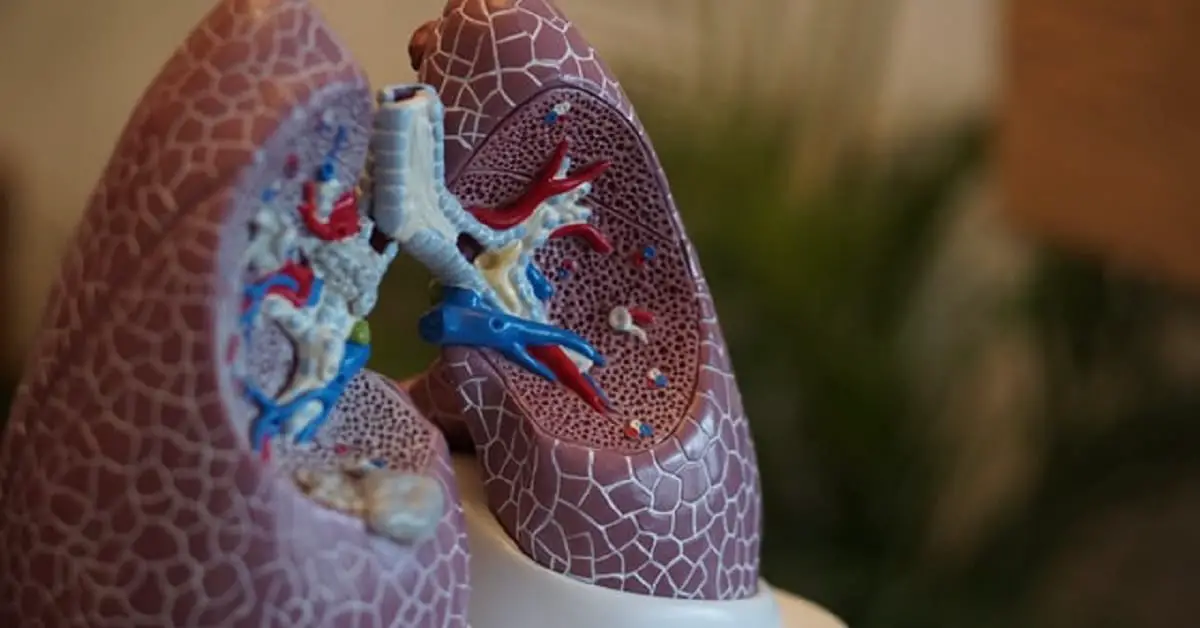
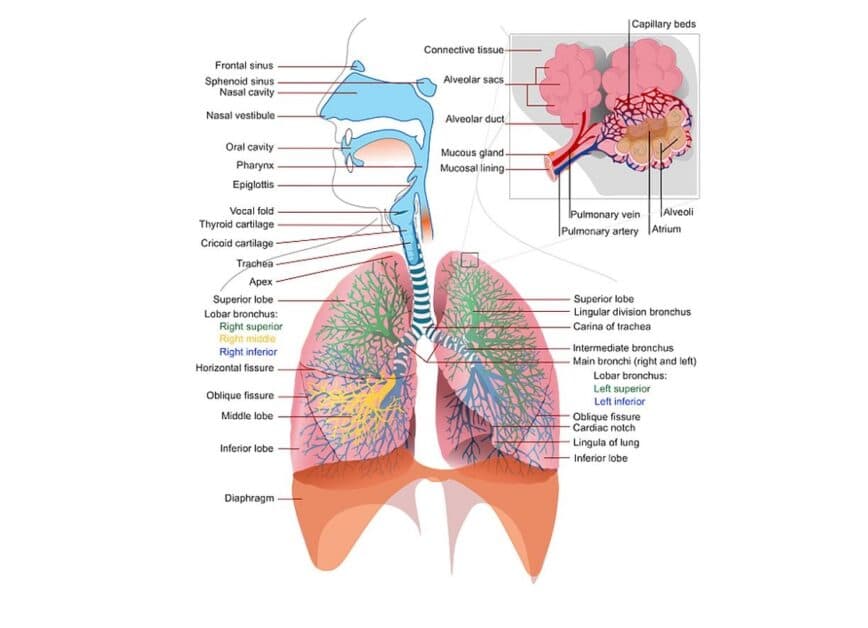
Alveoli are tiny balloon-shaped air sacs found at the end of the lung’s bronchioles (see image below). They are the place where your bloodstream takes in oxygen from the air you breathe in and releases carbon dioxide.
When the air sacs become filled with fluid due to infection, the lungs can’t work efficiently, and you may develop uncomfortable signs and symptoms of pneumonia, such as respiratory distress, coughing, chest pain, and fever.
Pneumonia infection often spreads from person to person through inhaling airborne droplets containing viral or bacterial pathogens deposited in the air by other infected people. It may also spread through people touching their eyes and nose after touching infected surfaces or objects.
People infected with the illness may be symptomatic or asymptomatic. Asymptomatic individuals may also spread the pathogens through droplets from their mouths when they speak, cough, or sneeze.
Pneumonia is a global health problem
Pneumonia is a public health threat worldwide and in the U.S. The disease affects people of all ages, and despite the availability of vaccines and antibiotics, pneumonia remains one of the top causes of illness that causes hospitalization and death.
The World Health Organization (WHO) reported that healthcare providers record about 450 million cases of pneumonia worldwide every year, and about 4 million die from the disease.
Pneumonia is a leading cause of mortality among the elderly and the top infectious disease cause of death among young children, according to the WHO. In 2019, the disease killed 740,180 children under 5, about 14% of all deaths in that age group.
About 5 to 10 million Americans develop pneumonia each year, with about 1 million hospitalized and about 70,000 dying, Rolston and Nesher reported.
If you’ve been searching for information about the signs and symptoms of pneumonia, then you’ve come to the right place.
This article answers all your questions about pneumonia, including causes, types, signs and symptoms, risk factors, how to prevent the disease, what to do if you fall ill with the disease, and more.
Symptoms of pneumonia in adults and children
Pneumonia causes inflammation and filling of the alveoli (the air sacs of the lungs) with pus (thick infected fluid), making it difficult for sufferers to breathe and get oxygen into their bloodstreams for distribution to the body tissues and organs.
Pneumonia localized to one or more lobes of a lung is called lobar pneumonia. Infection that spreads in patches across lung tissues without localization is called bronchial pneumonia or bronchopneumonia. However, it is often difficult in practice to distinguish between bronchial and lobar pneumonia.
The symptoms of pneumonia vary from case to case. Depending on the degree of severity of the infection, symptoms may vary from mild (similar to common cold or flu) to moderate and severe, with coughing, difficulty breathing, chills, and fever.
The severity of infection depends on many factors. Vitamin and mineral deficiencies — such as iron deficiency — may predispose to severe illness. The immune status of the patient, pathogen load, and age are also significant factors.
Infants, young children, and older people (>65 years old) are the most susceptible to severe pneumonia illness.
“Age is perhaps one of the most significant factors. Younger children are more susceptible and have more severe disease,” CARE healthy living Medical Advisor Dr. Moyo Adeyemi, FRCPC, explained. “Of course, we see more cases in winter due to RSV (respiratory syncytial virus), flu, and other less common respiratory viruses.”
Signs and symptoms of viral and bacterial pneumonia
The symptoms of bacterial and viral pneumonia may include:
- Cough may be productive in bacterial pneumonia and dry or unproductive in viral pneumonia, alongside flu-like symptoms. Coughing may produce bloody, yellow, greenish mucus or phlegm.
- Patients with bacterial pneumonia frequently experience fever and chills. Sweating may also be profuse.
- Headache is a common symptom of pneumonia
- Weakness, tiredness, fatigue, lethargy, and lack of energy
- Muscles and joints aches and pain
- Wheezing occurs more commonly in viral pneumonia
- Restlessness is also a common symptom
- Shortness of breath or rapid shallow breathing may occur
- Increased pulse rate
- Dyspnea or difficulty breathing
- Lips and nailbeds may have a bluish tinge due to a lack of oxygen
- Patients may complain of sharp or stabbing pain in the chest. Coughing and deep breathing may worsen the pain
- Loss of appetite or unwillingness to eat and drink may worsen weakness
- Nausea and vomiting occur, especially in infants and young children
- Diarrhea occurs in some cases
Signs and symptoms of pneumonia in adults

Adults, especially older adults (>65), may have different pneumonia symptoms.
Older people and others with a weak immune system may show mild symptoms of illness that mask the severity of the infection. Older patients may have low or normal temperatures even when they have severe, life-threatening sickness.
Confusion, delirium, and lowered alertness are signs that occur more commonly in older patients.
Symptoms of pneumonia in young children (<5 years)
- Runny or stuffy nose
- Sneezing
- Wheezing
- Watery eyes
- Sore throat
- Vomiting
- Diarrhea
Symptoms of pneumonia in infants
Infants may show no symptoms of infection, but they may also have the following:
- Fever
- Convulsions
- Cough
- Restlessness
- Lack of energy
- Respiratory distress
- Loss of appetite
- The skin may be blue-tinged
- Nausea and vomiting
- Diarrhea
- Decreased consciousness
[Note: Scroll down to read about the signs and symptoms of various types of pneumonia, including aspiration pneumonia, pneumococcal, mycoplasma, viral pneumonia, and Legionnaires disease.]
Pneumonia risk factors

Immune status and overall health is an important factor in the risk of developing pneumonia.
The elderly (>65 years) are at a higher risk of severe illness due to their decreased level of immunity. Infants and young children, 5 years old and younger, are also at higher risk of severe illness because their immune systems can’t effectively ward off infection.
“Children who live in poorer communities are more likely to be affected due to overcrowding,” Dr. Moyo Adeyemi said. “Children in areas (such as Northern Manitoba) with high MRSA (methicillin-resistant Staphylococcus aureus) prevalence are also more likely to get pneumonia.”
“Children with chronic conditions, especially congenital heart diseases or conditions that predispose to aspiration are also more susceptible to severe illness,” Dr. Adeyemi added. “Preterm babies are a huge group for obvious reasons. They are immunocompromised already and more likely to have issues like chronic lung disease or congenital heart conditions.”
Besides age, smokers and second-hand smokers, people with respiratory infections, such as common cold, flu, laryngitis, chronic lung and respiratory diseases, such as asthma, bronchiectasis, and chronic obstructive pulmonary disease (COPD), are all at a higher risk of developing severe illness because the preexisting conditions have weakened their ability to resist infection.
Any condition that weakens the immune system — poverty and poor nutrition (vitamin D deficiency, for instance), alcohol abuse, HIV/AIDS infection, cancer chemotherapy, surgery (organ transplant surgery), immunosuppressive medication — makes you more likely to suffer severe pneumonia.
Some studies suggested that medication such as proton pump inhibitors (PPIs) and histamine-type 2 receptor blockers (H2 blockers) increased the risk of pneumonia in stroke patients.
However, Dublin et al. concluded that PPIs and H2 blockers were not associated with increased pneumonia risk in older adults.
People with heart disease (including heart failure), kidney disease, liver disease, cystic fibrosis, diabetes, and sickle anemia, are also at risk of severe pneumonia.
Exposure to airborne irritants such as chemicals, toxic particles, and fumes increases the risk of illness.
Individuals with certain genetic conditions, such as TLR6 polymorphism, have an increased risk of contracting the form of pneumonia known as Legionnaires disease, Misch et al. reported.
Hospital-acquired pneumonia, HAP

Lynch noted that pneumonia complicates hospitalization in about 0.5%-2.0% of patients. Pneumonia contracted by individuals undergoing treatment, recuperating, or recovering from severe illness at a hospital is called hospital-acquired pneumonia (HAP) (also known as nosocomial pneumonia). Experts consider HAP a significant cause of sickness and death among certain hospitalized patients.
According to Shebl and Gullick, HAP is pneumonia that was not incubating at the time of admission and which the patient presents with at least two days (48 hours) after hospitalization. Cases that do not meet that criteria are considered community-acquired pneumonia (CAP).
Experts consider HAP a more serious infection than CAP because it often involves antibiotic-resistant pathogens attacking patients already weakened by illness.
Nichani et al. noted that one of the primary risk factors for HAP was mechanical ventilation and intubation during hospitalization. The authors estimated that HAP occurs in 9% to 27% of all patients intubated during hospitalization.
Ventilator-associated pneumonia (VAP) is a subset of HAP that occurs among patients admitted to ICUs. It is defined, according to Shebl and Gullick, as pneumonia that occurs 48-78 hours after tracheal intubation. Studies estimated that VAP affects about 10%-20% of patients receiving mechanical ventilation at the hospital.
HAP and VAP may be caused by gram-positive cocci, such as Staphylococcus aureus, and gram-negative bacilli, such as Escherichia coli, Enterobacter spp, Pseudomonas aeruginosa, and Klebsiella pneumoniae, Shebl and Gullick reported.
Healthcare-associated pneumonia (HCAP)

Experts distinguish between healthcare-associated pneumonia (HCAP) and HAP.
HCAP refers to pneumonia acquired by patients in “healthcare environments outside of the traditional hospital setting,” such as long-term care facilities, according to Nichani et al.
The American Thoracic Society (ATS) and Infectious Disease Society of America (IDSA) define HCAP as pneumonia that develops in patients during or after a stay at a healthcare facility, such as a nursing home or long-term care facility, home infusion therapy service, or chronic dialysis.
Aspiration pneumonia
Liquid, saliva, stomach acid and content, nasopharyngeal (area of the throat behind the nose) secretions, food, toxic, and non-toxic foreign material may sometimes pass from the mouth or upper gastrointestinal tract into the airway or lungs.
It may lead to inflammation or infection of the airway and lungs, leading to a condition known as aspiration pneumonia.
Aspiration pneumonia may also lead to complications, such as acute respiratory distress syndrome (ARDS).
People most susceptible to aspiration pneumonia include:
- Individuals weakened by chronic illness
- Old age-related frailty and debility
- People who abuse drugs or alcohol
- Individuals experiencing altered mental states, or individuals who aren’t fully alert or conscious due to sedatives or general anesthesia administered for surgery
- Patients with dysphagia or swallowing dysfunction due to chronic obstructive pulmonary disease (COPD) or neurologic diseases, such as dementia, Parkinson’s disease, multiple sclerosis, and stroke, according to Son et al.
- Individuals with disorders of the esophagus
- People with gastrointestinal disorders
- Patients placed on gastric feeding tubes may develop aspiration pneumonia
Symptoms of aspiration pneumonia
According to Son et al., aspiration pneumonia may cause the following symptoms:
- Hypoxemia (low concentration of oxygen in the blood)
- Fever
- Tachycardia (abnormally fast heart rate)
- Abnormalities in chest radiograph
- Persistent cough
- Fatigue
- Dyspnea
What causes pneumonia?
Pneumonia is caused by infection of the lungs by viral, bacterial, or fungal pathogens.
Community-acquire pneumonia (CAP) is the most common form. As the name implies, CAP is pneumonia contracted through transmission within a community.
The pathogens that cause pneumonia may reach the lungs through various means, but often through inhaling contaminated airborne droplets or aerosols into the upper respiratory tract and then aspiration of pathogens residing in the upper respiratory tract (nose and throat) into the lower respiratory tract and the lungs.
Pneumonitis refers to non-infectious inflammation of the lungs caused by agents, such as medication, allergens, chemicals, and pollutants.
Bacterial pneumonia
Bacterial pneumonia is the most common type and often the most severe. It often occurs as a complication of preexisting respiratory viral infection in patients with lowered immunity.
The bacterial pathogen Streptococcus pneumoniae causes pneumococcal pneumonia, one of the most common types of bacterial pneumonia. Pneumococcal pneumonia causes about 150,000 hospitalizations every year in the United States, according to CDC. The disease kills about 5% of people who get it.
Symptoms of pneumococcal pneumonia
According to CDC, pneumococcal pneumonia may cause the following signs and symptoms:
- Fever
- Chills
- Cough
- Rapid breathing or difficulty breathing
- Chest pain
- Older patients may experience confusion or lowered alertness.
- Patients with pneumococcal pneumonia may have bloody or rust-colored sputum (hemoptysis)
Other bacterial pathogens that may cause pneumonia include gram-positive and gram-negative organisms such as Staphylococcus aureus, Haemophilus influenzae, Pseudomonas aeruginosa, Acinetobacter baumannii, Escherichia coli, Klebsiella pneumoniae, and Moraxella catarrhali.
People with pneumonia caused by Klebsiella may also have bloody “currant jelly” sputum.
Mycoplasma pneumonia, also referred to as “walking pneumonia,” affects younger people exposed to crowded conditions. It causes a mild — but occasionally serious — infection of the respiratory system that may go undiagnosed for many years.
Symptoms of Mycoplasma pneumonia
Signs of symptoms of Mycoplasma pneumonia (“walking pneumonia”) may include:
- Joint pains
- Swelling of the lymph nodes
- Middle ear infection
According to the CDC, they may also include symptoms of a chest cold, such as:
- Sore throat
- Weakness and lethargy
- Fever
- Cough
- Headache
Chlamydia pneumoniae causes respiratory tract infection and pneumonia. Some infected people show no symptoms or only mild symptoms.
Legionella pneumophila causes Legionnaires disease, a severe pneumonia usually contracted through exposure to contaminated water and water systems.
Symptoms of Legionnaires disease
Symptoms of Legionnaires disease may include
- Diarrhea
- Nausea
- Abdominal pain
- Confusion
Viral pneumonia
Viral pneumonia often occurs in people with preexisting respiratory and lung diseases, and people with chronic illnesses, such as heart disease.
It is usually caused by viruses that infect the upper respiratory tract, such as influenza viruses, respiratory syncytial virus (RSV) (more common in children), and COVID-19 virus SARS-CoV-2 (more common in adults).
Other viruses that may cause pneumonia include rhinoviruses, adenovirus, parainfluenza, and cytomegalovirus.
Pneumonia caused by SARS-CoV-2 (coronavirus) could result in life-threatening respiratory illnesses. It is behind many news reports of respiratory emergencies associated with COVID-19 sickness that makes doctors place patients on ventilators. The viral infection of the lungs leads to inflammation and fluid filling the lungs, causing respiratory distress. Acute respiratory distress syndrome (ARDS) caused by the SARS-CoV-2 virus may lead to respiratory failure and death.
Sometimes viral pneumonia is complicated by a secondary bacterial infection, such as Streptococcus pneumoniae, Staphylococcus aureus, or Haemophilus influenzae.
Symptoms of viral pneumonia
Signs and symptoms of viral pneumonia may include:
- Headaches
- Shortness of breath
- Muscle aches and pain
- Weakness and general malaise
- Wheezing occurs more commonly in viral pneumonia
- Cough gets worse over time and maybe dry or unproductive
Fungal pneumonia
Fungal pneumonia is less common than the other types of pneumonia. It is more likely to occur in people with longstanding illnesses and immunocompromised people, such as HIV/AIDS patients and people on immunosuppressive medication.
- Pneumocystis pneumonia (PCP) is a potentially serious fungal infection of the lungs caused by Pneumocystis jirovecii. It typically affects people with weakened immunity.
- Cryptococcus neoformans also usually infects people with a weakened immune system. Healthy people exposed to it usually don’t get sick.
- Coccidioidomycosis is caused by Coccidioides immitis or C. posadasii. It is also known as valley fever. It is common in the southwestern U.S. and Northern Mexico.
- Histoplasmosis is caused by a fungus called Histoplasma capsulatum. It is found in the Mississippi River Valleys and Ohio.
- Blastomycosis is caused by breathing in the microscopic fungal spores of fungus Blastomyces, found in moist soil and decomposing organic matter in parts of the U.S., including Ohio, Mississippi River valleys, and the Great Lakes.
Complications of pneumonia

A complication is any problem or change that arises during an illness that may worsen prognosis (likely culmination of a disease).
Complications that may arise in pneumonia include:
- Acute respiratory distress syndrome (ARDS) may lead to respiratory failure. Patients often require mechanical ventilation.
- Bacteremia happens when bacteria enter the bloodstream. It is a dangerous condition because it can lead to sepsis and septic shock
- Pericarditis refers to inflammation of the membrane (pericardium) that surrounds the heart
- Lung abscesses and necrosis (death) of pulmonary (lung ) tissues due to microbial infection. Necrosis causes cavities within the lungs and accumulation of debris and fluid that may complicate pneumonia and increase the risk of poor disease outcome
- Bronchial obstruction: Blockage or obstruction of the airway leading to collapse (atelectasis).
- Post-obstructive pneumonia is often seen in cases of malignancy but also occasionally in patients with CAP
- Pleural disorders may affect the space between the thin, membraneous tissues (pleura) that line the lungs and the inside of the chest cavity. Pleural disorders may involve inflammation (pleurisy), infection, or injury that causes the pleural space to become filled with excess fluid, blood, pus (pleural effusion), or air, and gas (pneumothorax).
- Kidney failure is another possible complication of pneumonia, according to CDC
When to call your doctor
Pneumonia is a serious illness with potentially life-threatening complications, so don’t hesitate to seek medical help if you believe that you, your child, or a relative is showing symptoms that could be due to pneumonia.
Pneumonia could be difficult to diagnose partly because the severity of the infection is not always obvious at first. Initial symptoms are often mild and similar to those of cold or flu.
Only a doctor can diagnose the disease based on your recent contacts, medical history, and symptoms. He may conduct a physical examination, order a chest x-ray, CT scan, blood, and sputum tests.
It is dangerous to delay while trying to self-diagnose or self-medicate if you believe you may have the illness.
Danger signs and symptoms of pneumonia

Danger signs and symptoms of pneumonia that may indicate you need to seek medical attention immediately include:
- High fever
- Respiratory distress
- Bluish color in nailbeds or lips
- Severe cough with thick mucus
- Chest pain
If you are diagnosed with pneumonia, you must strictly follow your doctor’s recommendation and take your medication as prescribed. You also need to follow medical advice to rest during recovery and recuperation.
Treatment of pneumonia depends on the pathogen responsible for the illness and the severity of the infection. Usually, patients with severe illness will be hospitalized. Your doctor may prescribe antibiotics to treat bacterial pneumonia.
How to prevent pneumonia
A healthy diet, lifestyle, and strict hygiene strengthen the immune system’s ability to fight off infections. Avoid smoking because it weakens and damages the lungs, making you more susceptible to infection. Also, avoid alcohol and drugs that may leave you open to infection by lowering your immunity.
Hygiene will involve washing your hands frequently. You also need to practice social distancing by avoiding being around people who may have the infection, especially if you are at high risk.
You can avoid contracting pneumonia by getting vaccinated against bacteria and viruses that cause the disease. You may lower your risk of getting pneumonia by vaccinating against the following diseases:
- Haemophilus influenzae type b (Hib)
- Influenza (flu)
- Pertussis (whooping cough).
- Measles
- Pneumococcal Pneumonia
- Varicella (chickenpox)
- COVID-19 vaccination
[Featured image: Robina Weermeijer/Unsplash.com]